The initial medical assessment and subsequent diagnostic tests for burns are critical in providing effective treatment and care for burn victims. These procedures involve a thorough evaluation of the burn’s degree, skin thickness, and extent, which are essential for understanding the severity of the injury and determining the best course of action. Employing diagnostic tests for burns, such as the Rule of Nines or the Lund and Browder chart, allows clinicians to estimate the total body surface area affected and tailor treatments to individual patient needs. Furthermore, the comprehensive approach extends beyond physical assessment to include a detailed patient history, which reveals any pre-existing conditions or medications that could influence recovery. This holistic evaluation is vital for devising a strategic care plan that addresses both the immediate and long-term needs of burn patients.
Initial Medical Assessment
The initial medical assessment of burns is a critical component of emergency care, essential for determining the appropriate treatment and intervention strategies. Conducting a thorough physical examination of the burn patient allows clinicians to accurately assess the depth and extent of burns, which are pivotal in guiding therapeutic decisions.
Firstly, assessing burn depth involves examining the affected skin to determine whether the burn is superficial, partial-thickness, or full-thickness. This assessment influences both immediate treatment options and long-term healing prospects. Moreover, evaluating the extent of the burn, typically through the Rule of Nines or the Lund and Browder chart, helps in estimating the percentage of total body surface area affected—a crucial factor in formulating resuscitation protocols and managing potential complications.
In addition to the physical examination:
- Clinicians must look for associated injuries, such as inhalation injuries, fractures, or other trauma that often accompany severe burns.
- Careful inspection for signs of complications like infection or shock is vital, especially in extensive burns.
Obtaining a comprehensive patient history is equally important. This includes documenting the mechanism of injury to understand the circumstances leading to the burn, which provides insights into potential complications such as chemical exposure or an electrical injury’s systemic effects.
Key aspects of patients’ history should also cover:
- Any pre-existing medical conditions that might affect recovery, like diabetes or cardiovascular diseases.
- Current medications that could influence treatment choices, such as anticoagulants that increase bleeding risks.
- Allergies to medications, which are critical in avoiding adverse reactions.
Utilizing Burn Severity Scales
In clinical practice, accurately assessing the severity of burns is pivotal for effective treatment and management. Several burn severity scales are utilized to guide clinicians in their initial assessments and subsequent treatment strategies. Among these, the most commonly used are the Total Body Surface Area (TBSA) percentage, the Rule of Nines, and the Lund and Browder chart.
The TBSA percentage is crucial for determining the extent of burns. It assists in calculating fluid resuscitation needs, which is vital for preventing shock in burn patients. This scale is applied by estimating the percentage of the skin surface that has been burned, guiding both immediate and long-term treatment plans.
The Rule of Nines is an efficient method for quick estimation during initial assessments. It divides the body into sections that represent approximately 9% or multiples thereof of the body surface area. This tool is particularly useful in adult patients for rapid assessment in emergency settings.
Conversely, the Lund and Browder chart offers more precision than the Rule of Nines, especially beneficial in pediatric patients, as it accounts for the proportional differences in body surface area with age. It adjusts the percentage values of various body parts, providing a more accurate assessment for young children.
Additionally:
- Each scale plays a vital role in the triage process, helping to classify burns as minor, moderate, or severe based on the depth and extent of the injury.
- Clinicians also use these scales to monitor the progression of treatment and adjust interventions as needed.
Employing these burn severity scales allows for standardized assessments across different clinical settings, ensuring that patients receive appropriate and consistent care tailored to the severity of their injuries. This systematic approach not only improves immediate response but also enhances long-term recovery outcomes for burn victims.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
Diagnostic Procedures for Burns
Diagnostic procedures for burns are crucial in assessing the extent and severity of injuries, providing essential data to guide effective treatment strategies. These evaluations, which include a range of laboratory tests and specialized assessments, are vital in understanding the impact of burns on skin thickness, the degree of damage, and overall patient care. By measuring various biomarkers, clinicians can detect physiological changes and potential complications, ensuring that each patient receives personalized medical attention. From routine blood tests that monitor hematologic status and electrolyte balance to more specialized tests for lactate levels and carbon monoxide exposure, each diagnostic tool plays a critical role in the comprehensive care and management of burn wounds. This systematic approach allows for continuous evaluation, helping to adapt treatments as the patient’s condition evolves and ensuring optimal recovery outcomes.
Laboratory Tests
In the management of burn injuries, diagnostic procedures, particularly laboratory tests, play a crucial role in assessing the severity and guiding treatment strategies. These tests are essential for monitoring the physiological effects of burns and for detecting complications early in the treatment process.
Initially, a complete blood count (CBC) is performed to evaluate the patient’s hematologic status. This test helps in identifying anemia or signs of infection through elevated white blood cell counts. Additionally, electrolyte and fluid balance are monitored closely with serum electrolyte tests, as burns can lead to significant shifts in potassium, sodium, and other critical electrolytes.
Renal function tests, including blood urea nitrogen (BUN) and creatinine, are essential, particularly in patients with large burns, to assess the impact of burn shock on renal perfusion and function. These parameters indicate the adequacy of fluid resuscitation and the potential need for adjustments in therapy.
Moreover:
- A coagulation profile is necessary to detect any disseminated intravascular coagulation (DIC), a possible complication in severe burns.
- Arterial blood gasses (ABG) are measured to assess oxygenation and carbon dioxide removal, crucial for patients who have inhalation injuries or respiratory distress.
Clinicians also utilize serum lactate levels to evaluate the severity of shock and perfusion status. An elevated lactate can indicate inadequate tissue oxygenation, prompting more aggressive fluid and oxygen therapy.
These laboratory tests are integral components of the initial and ongoing assessment of burn patients. They provide valuable information that impacts clinical decisions regarding fluid management, respiratory support, and potential interventions to prevent renal failure and other complications. Through systematic and repeated evaluation using these tests, clinicians can effectively monitor the progression of recovery and adjust treatments as the patient’s condition evolves.
Biomarkers and Specialized Tests
In the specialized management of burn injuries, clinicians rely on a range of biomarkers and laboratory tests to assess burn severity and identify potential complications. Among the crucial tests are measurements of lactate levels, carbon monoxide levels, and carboxyhemoglobin levels, each providing insights into the patient’s physiological state and guiding treatment decisions.
Lactate levels are a key indicator of tissue hypoxia and metabolic stress. Elevated lactate suggests that tissues are not receiving enough oxygen, a common issue in severe burn cases where circulation may be compromised. Monitoring these levels helps clinicians assess the effectiveness of resuscitation efforts and make necessary adjustments to fluid therapy and oxygen delivery.
Carbon monoxide (CO) poisoning is a serious concern in patients exposed to smoke or fires in enclosed spaces. Measuring carbon monoxide levels in the blood is critical for these patients, as CO binds to hemoglobin more effectively than oxygen, reducing the blood’s oxygen-carrying capacity. Symptoms of CO poisoning can be non-specific and include headache, dizziness, and nausea, underscoring the importance of this test in the diagnostic process.
Carboxyhemoglobin, a complex of carbon monoxide and hemoglobin, is another vital biomarker. Elevated levels indicate significant exposure to carbon monoxide, necessitating immediate intervention. Treatment typically involves administering 100% oxygen or using hyperbaric oxygen therapy to displace CO from hemoglobin, thus restoring its ability to transport oxygen.
These specialized tests are integral to the comprehensive care of burn patients, enabling clinicians to diagnose critical conditions quickly, adjust treatments, and potentially prevent life-threatening complications. By continuously monitoring these biomarkers, healthcare providers can significantly improve outcomes for burn victims, emphasizing the necessity of these assessments in modern burn care protocols.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
Imaging Modalities in Burn Diagnosis
Radiographic imaging is indispensable in the thorough evaluation and management of burn injuries, playing a pivotal role in both initial diagnosis and ongoing monitoring. Utilizing a range of technologies such as X-rays, ultrasound, and computed tomography (CT) scans, clinicians can uncover not only the superficial extent but also the deeper implications of burns. These imaging tools are critical for detecting hidden injuries such as fractures and internal organ damage, ensuring a comprehensive assessment that informs targeted treatment strategies. Each modality offers unique benefits, from the rapid screening capabilities of X-rays to the detailed anatomical insights provided by CT scans, enhancing the care and management of patients with burn injuries.
Radiographic Imaging
Imaging modalities play a critical role in the comprehensive evaluation of burn injuries, particularly when assessing for associated trauma that might not be immediately apparent. X-rays, ultrasound, and computed tomography (CT) scans are among the primary tools utilized by clinicians to gain deeper insights into the extent and nature of burn-related damage.
X-rays are typically the first-line imaging tool for identifying underlying fractures or inhalation injuries. They are especially useful for detecting rib fractures or pneumothoraces that can complicate the clinical picture in cases of severe burns. This quick and widely available modality helps to confirm the presence of foreign objects or bone abnormalities that require immediate attention.
Ultrasound imaging provides a non-invasive means to assess soft tissue structures around the burn area. This modality is beneficial for guiding fluid drainage procedures and evaluating the depth of burn injuries more precisely, without the need for radiation exposure. It can reveal fluid collections that might otherwise be missed during a routine physical examination.
Furthermore, CT scans offer a more detailed view of the internal anatomy, allowing clinicians to assess the full extent of trauma, including deeper tissue damage and organ involvement in burn patients. CT imaging is particularly valuable in planning surgical interventions, such as debridement and reconstruction, by providing high-resolution images of bone and soft tissue.
- Each of these imaging modalities serves a unique purpose:
- X-rays pinpoint skeletal injuries and assess lung health.
- Ultrasound evaluates soft tissue and fluid status in real-time.
- CT scans deliver comprehensive details on both soft tissue and bone structures.
Incorporating these imaging techniques into the diagnostic process enhances the accuracy of assessments, guides therapeutic decisions, and ultimately improves patient outcomes by ensuring all injuries—visible and hidden—are adequately addressed.
Thermal Imaging and Advanced Techniques
Emerging technologies such as thermal imaging and laser Doppler imaging are revolutionizing the assessment of burn depth and extent, providing clinicians with advanced tools to enhance accuracy in diagnosis and treatment planning. Thermal imaging utilizes infrared technology to detect heat patterns emitted from the skin’s surface. This method enables a quick visual assessment of the burn area, highlighting variations in skin temperature that correlate with the severity and depth of burns. It is particularly useful in differentiating between superficial and deeper burns, facilitating timely and appropriate treatment interventions.
Laser Doppler imaging, another innovative technique, measures blood flow in the microcirculation of burned skin. By projecting a low-intensity laser onto the skin and analyzing the Doppler shift of light reflected from moving red blood cells, this technology provides quantitative data on tissue perfusion. Areas with reduced or no blood flow indicate deeper tissue damage, crucial for surgical planning, such as determining the need for excision and grafting.
Furthermore:
- These technologies offer non-contact, pain-free assessment methods that reduce discomfort for burn victims during evaluations.
- They allow for repeated assessments without risk to the damaged tissues, providing dynamic information about the healing process and guiding ongoing treatment decisions.
Adopting these advanced imaging modalities in clinical settings not only enhances diagnostic precision but also improves patient outcomes by ensuring targeted and effective treatment strategies. As these technologies continue to develop, they promise to become integral components of modern burn care, pushing the boundaries of what is possible in both assessment and management of burn injuries.
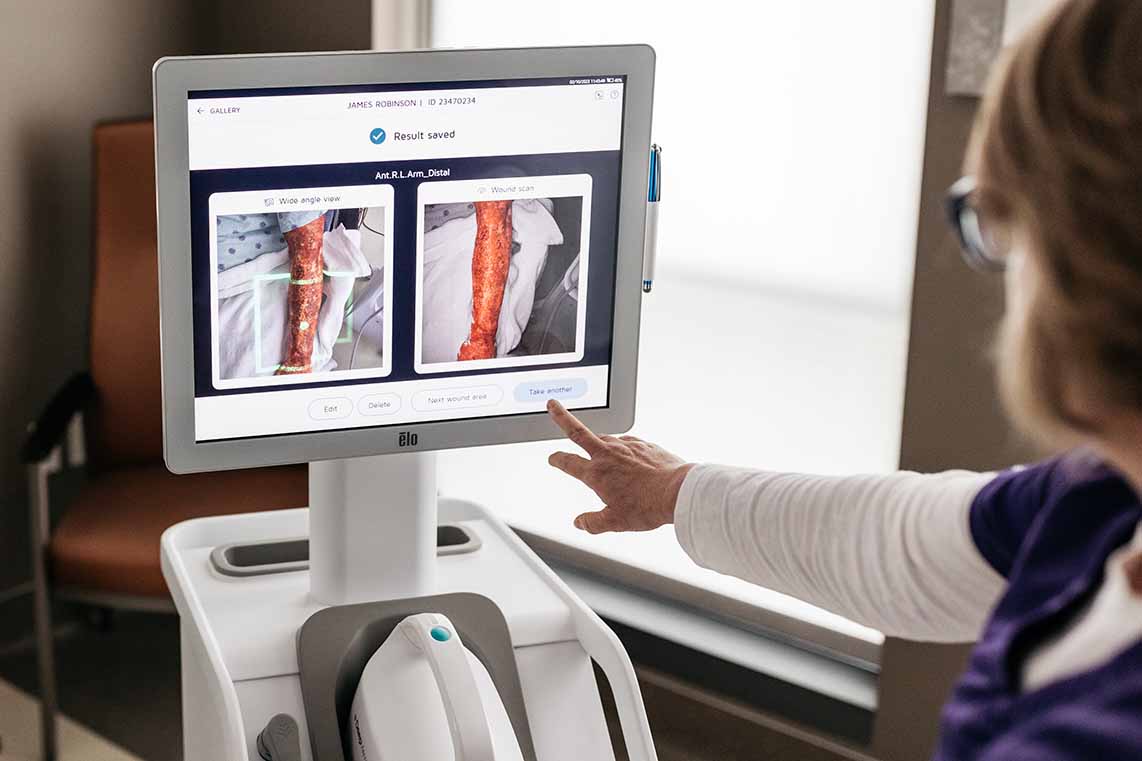
Deepview
Our patented DeepView® technology is an AI wound diagnostics platform that combines AI algorithms and medical imaging for diagnostic wound healing predictions.
DeepView® provides clinicians with a ‘Day One’ wound healing assessment that enables the clinician to triage the patient to the appropriate care setting sooner.
DeepView®’s current accuracy in determining healing or non-healing burn wounds is 92%, compared with current physician accuracy of 50 to 70%.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?
Patient Care and Treatment Strategies
Effective management of burn injuries involves a holistic approach that incorporates a multidisciplinary team of healthcare professionals. This team, which includes burn surgeons, nurses, physical therapists, nutritionists, and psychologists, collaborates to provide comprehensive care tailored to each patient’s specific needs. From the initial assessment of the burn’s degree, thickness, and overall impact on the skin, to continuous monitoring and follow-up, the focus is on both the physical healing of the wounds and the overall well-being of the patient. This approach ensures that all aspects of recovery, from wound management to psychological support, are addressed, creating a foundation for successful healing and long-term recovery.
Multidisciplinary Approach to Burn Care
The treatment of burn injuries requires a comprehensive, multidisciplinary approach to ensure optimal recovery for patients. This strategy involves a team of specialists, including burn surgeons, nurses, physical therapists, nutritionists, and psychologists, each playing a vital role in patient care.
Initially, burn surgeons and nurses collaborate to provide immediate care, focusing on stabilizing the patient, assessing burn depth and extent, and managing pain and infection risks. The early stage of treatment often involves fluid resuscitation, wound cleaning, and the application of dressings to protect the burn surface and promote healing.
As the patient progresses:
- Physical therapists design rehabilitation programs to restore mobility and prevent contractures, essential for maintaining functional abilities and enhancing quality of life.
- Nutritionists are integral, developing tailored dietary plans to meet the increased metabolic demands of burn recovery, ensuring patients receive adequate calories and nutrients to support tissue repair and immune function.
Additionally, psychologists support emotional and psychological recovery, addressing common issues such as trauma, anxiety, and depression that often follow serious burn injuries. Their role is crucial in helping patients cope with the long-term impacts of their injuries, including scarring and potential changes in body image.
Moreover, regular multidisciplinary team meetings facilitate the integration of care, allowing for ongoing assessment and adjustment of treatment plans based on the patient’s recovery status. This cohesive approach ensures that all aspects of the patient’s health are considered, leading to more personalized and effective treatment strategies.
Ultimately, a multidisciplinary approach in burn care not only focuses on the immediate physical healing but also encompasses the overall well-being of the patient, setting a foundation for successful long-term recovery. Through coordinated efforts, the care team maximizes the potential for positive outcomes, addressing both medical and psychosocial needs comprehensively.
Treatment Planning
Treatment planning for burns is a meticulous process that requires a detailed evaluation of the burn’s degree, thickness, and overall impact on the skin. This strategy ensures that each patient receives personalized care tailored to the specific characteristics of their injury.
Initially, clinicians assess the degree of burns by examining the depth and extent of skin damage. This evaluation helps determine whether the burns are superficial, partial thickness, or full thickness, each requiring different treatment approaches. Superficial burns might need only minimal treatment such as cooling and simple dressings, while full-thickness burns could require surgical interventions like debridement or skin grafting.
Moreover, the overall plan incorporates a comprehensive wound management strategy to promote healing and prevent infection. Key components include:
- Regular cleaning of the wound to remove debris and prevent bacterial growth.
- Applying appropriate dressings that maintain a moist environment conducive to healing.
- Monitoring for signs of infection or complications that may necessitate adjustments in treatment.
In addition to wound care, the treatment plan also addresses pain management and nutritional support, crucial for enhancing the patient’s comfort and supporting the body’s healing capacity. Rehabilitation services are integrated early in the planning to ensure that the patient maintains mobility and functionality, especially in cases where large areas of skin are affected.
Regular follow-ups and reassessments are essential parts of the treatment plan, allowing healthcare providers to track the healing progress and make necessary modifications. This adaptive approach helps in effectively managing the patient’s recovery, ensuring that the treatment remains aligned with their evolving needs.
Monitoring and Follow-Up
Ongoing monitoring and follow-up are critical components of effective burn care, ensuring that treatments are successful and complications are promptly addressed. Regular assessments allow healthcare providers to evaluate the healing progress of burns, adapt treatment plans as necessary, and ensure that patients receive the highest standard of care.
Initially, the severity and degree of burns determine the immediate treatment approach. As the patient progresses, continuous monitoring becomes essential to observe the skin’s recovery and identify any signs of infection or delayed healing. This step is crucial since the skin, the body’s first defense against infection, is compromised in burn injuries.
Follow-up visits are structured to assess not only the physical aspects of burn recovery but also to evaluate the patient’s overall well-being. During these visits:
- Clinicians review the condition of the healed and healing skin, checking for proper wound closure and any abnormal scar formation, which can be particularly challenging with third-degree burns.
- They also monitor for any functional impairments or mobility issues that might develop as a result of the skin and tissues becoming tighter or scarred.
Additionally, these sessions provide an opportunity to adjust pain management strategies and update rehabilitation exercises that are vital for recovery. Psychological support continues to be an integral part of follow-up care, helping patients cope with the mental and emotional impacts of burn injuries.
In conclusion, the assessment and treatment of burn injuries demand a meticulous and multidisciplinary approach that spans from immediate medical evaluation to long-term care strategies. The integration of various diagnostic tests for burns, including both physical examinations and laboratory assessments, is crucial for accurately gauging the severity of burns and optimizing patient outcomes. Each step, from the initial medical assessment to ongoing monitoring and follow-up, plays a vital role in ensuring comprehensive care. Utilizing severity scales and advanced imaging techniques helps tailor treatments to individual patient needs, thereby enhancing the effectiveness of medical interventions. Ultimately, the goal is to not only heal the physical wounds but also to address the psychological impacts, ensuring a holistic recovery for burn victims. This integrated approach underscores the complexity of burn care and the necessity of specialized knowledge and skills in managing these challenging injuries effectively.
More about Deepview
Learn more about our DeepView® technology
Request a Demo
Looking to learn more about DeepView® technology, or eager to see it in action?